PCOS: a common condition that deserves better understanding
PCOS affects around 1 in 10 women in the UK. Learn what PCOS is, common symptoms, diagnosis, fertility impact, and when to seek help.
Egg reserve, also known as ovarian reserve, refers to the number of eggs remaining in the ovaries. Egg reserve testing does not predict whether you will conceive naturally, but it provides helpful information about egg quantity. These tests are commonly used to support fertility planning, guide treatment options, and help individuals make informed decisions about their fertility.
Women are born with all the eggs they will ever have. Over time, both the number and quality of eggs decline, with a more noticeable drop from early 30’s, and rapid drop in mid-late 30’s and early 40’s. Unlike sperm, which are produced continuously, eggs are not replaced.
Egg reserve matters because it reflects how many eggs are left in your ovaries, helps guide treatment options such as ovulation induction, IVF/ICSI or donor eggs and predicts how your ovaries may respond to fertility treatment medications.
Egg reserve doesn’t predict the exact moment of menopause, but very low AMH can suggest a shorter remaining fertile window and a higher risk of early ovarian insufficiency and hence helps you plan your fertility realistically rather than rely on guesswork.
It is important to separate two concepts that are often confused:
Current egg reserve tests assess egg quantity only. They cannot measure egg quality or guarantee pregnancy outcomes.
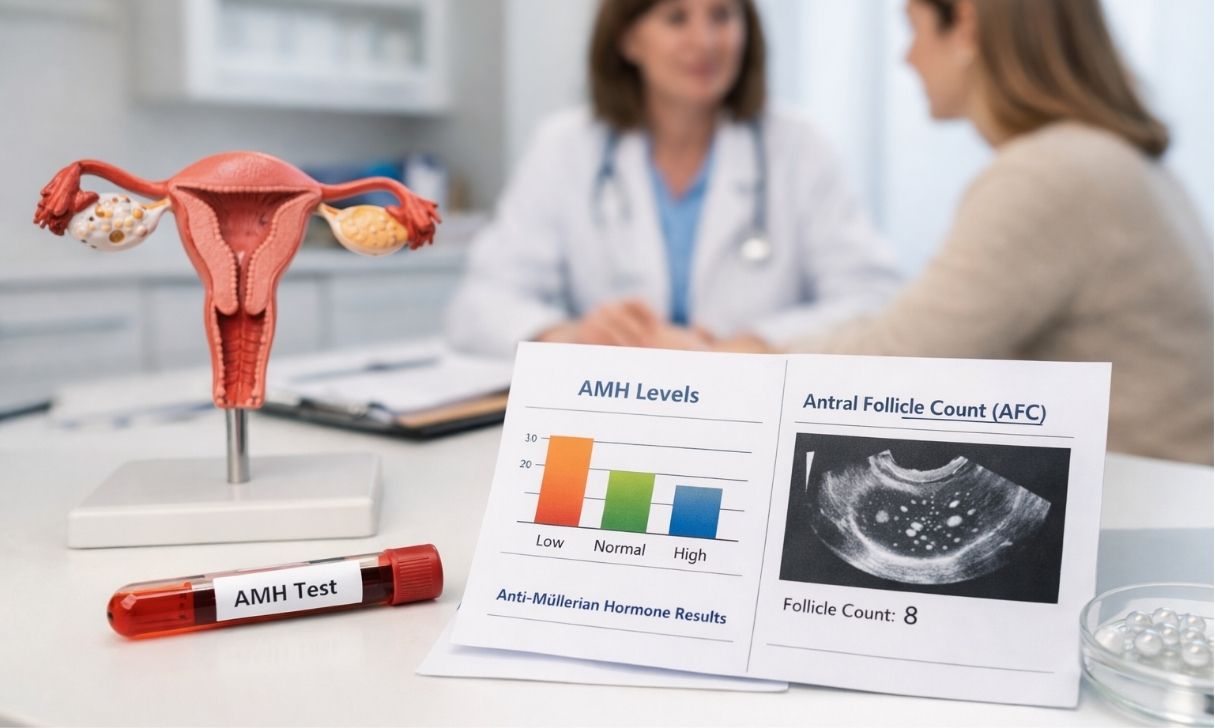
Egg reserve markers can be assessed by a blood test and by undertaking an ultrasound scan of your pelvis and ovaries. Testing for anti-mullerian hormone (AMH) by a blood test and assessing antra follicle count (AFC) on pelvic ultrasound scan together gives the most accurate picture of your egg reserve. Occasionally, a blood test for follicle stimulating hormone (FSH) and oestradiol (E2) is required to assess ovarian effort and baseline function
At JIVA Fertility, egg reserve assessment is often discussed during your fertility consultation and some times as part of recurrent miscarriage evaluation.
AMH stands for Anti-Müllerian Hormone. It is produced by very tiny follicles (egg containing sacs) in the ovaries that contain immature eggs. The level of AMH in the blood reflects the overall pool of eggs available. AMH is widely recognised as a useful marker of egg reserve. In some areas in the UK this test is not available on the NHS.
A lower AMH level suggests a reduced pool of eggs, while a higher level suggests a larger reserve. However:
According to NICE guidance, AMH is primarily used to predict how the ovaries may respond to stimulation during IVF rather than the likelihood of pregnancy.*
An antral follicle count is measured during a transvaginal ultrasound scan. The clinician counts small follicles measuring around 2–8 mm in each ovary. These follicles represent eggs that are available in the current cycle, out of which one follicle (dominant follicle) is recruited to release the egg.
AMH reflects the overall egg pool, while AFC shows what is happening in the ovaries at that moment. Together, they provide a clearer and more reliable assessment and are commonly used when planning IVF/ICSI, egg freezing, or ovulation induction.
FSH, or follicle-stimulating hormone, is released by the pituitary gland to stimulate the ovaries. It is assessed by a blood test done on day 2–5 of the menstrual cycle. High FSH suggests that the ovaries are working harder to stimulate follicles and hence suggestive of lower reserve.
For these reasons, NICE guidance no longer recommends FSH as the primary test of ovarian reserve.*
Egg reserve tests are tools for planning, not predictions.
They can help answer questions such as:
They cannot tell you whether you will conceive naturally, as fertility depends on many factors including sperm health, fallopian tubes, ovulation, and overall health.
For many patients, these tests provide reassurance and clarity, allowing informed decisions rather than uncertainty.
NICE fertility guidelines (CG156) state that AMH and AFC are used to predict ovarian response during IVF, not to predict natural conception.*
Some NHS-funded IVF pathways include minimum AMH or AFC thresholds as part of eligibility criteria, although these vary by region.*
The UK fertility regulator reports increasing use of IVF and egg freezing, particularly among women in their 30s, reflecting later family planning trends.*
A: There is no test that gives an exact egg count. AMH and AFC provide estimates of egg quantity but not an exact number.
A: AMH levels naturally decline with age. What matters most is how your result is interpreted in context rather than a single number.
A: No. These tests do not predict natural pregnancy. They are mainly used to guide fertility treatment planning.
A: This can be helpful if you are over 30, planning to delay pregnancy, or considering fertility preservation, but it is best discussed with a fertility specialist.
A: AMH testing may be offered on the NHS in specific circumstances, but access varies by region.
If you are considering egg reserve testing or would like personalised advice, a fertility consultation can help place results in the right clinical context.
You may also find it helpful to read:
To discuss your options, you can book a fertility consultation or book an appointment directly.
Disclaimer: This article is intended for educational purposes and does not replace individual medical advice. Please consult a healthcare provider for assessment and treatment decisions.

PCOS affects around 1 in 10 women in the UK. Learn what PCOS is, common symptoms, diagnosis, fertility impact, and when to seek help.

Wondering when to start trying for two or more children? Learn how age, fertility and spacing affect family planning, with expert-backed UK advice and guidance.